Delivering COVID-19 Information across the Digital Divide
Organization : Monash University
Project Overview
Project Summary
Rural communities in Bangladesh and India where internet access is low but mobile phone access is high were targeted with text messages and personalized phone calls about COVID-19 preventative measures.
Impact
Receiving personal phone calls, with or without text messages, increased self-reported compliance with a prescribed set of health guidelines by up to 2.7 standard deviations relative to those who received text messages alone. Adding text messages with phone calls increased the impact by about 0.4-0.6 standard deviations.
Cost
Less than 10 cents (USD) per call to a rural household
Source
Source
Challenge
Effective communication of the life-saving instructions related to COVID-19 can counter misinformation and encourage individuals to seek more health information, adopt positive health behaviors, comply with prescribed behavior, and take the initiative to seek medical help when needed. The extremely transmissible nature of the virus forced countries around the world to adopt strict mobility restriction policies at the national and community levels for infection prevention and control (IPC). Parallel to these macro-level policies, individuals were prescribed to adopt precautionary and protective health behaviors such as regular handwashing, coughing and sneezing etiquette, wearing face masks, and following social distancing measures. Despite these measures, over 58 million people contracted COVID-19 and 1.3 million lost their lives to coronavirus in the first 11 months of its outbreak.
In rural communities of low-income countries, exposure to COVID-19 misinformation combined with low levels of education, poor health literacy, and other poverty and social disadvantages makes IPC more difficult, and aggravates the health crisis. To limit the spread of COVID-19, government agencies and non-government organizations (NGO) around the world are doing their best to communicate verified information and combat myths about the disease. However, there is still a significant digital divide in low-income countries; rural communities are less connected or disconnected from the digital world—an important source of health information, especially during the pandemic. Low-income countries must find other ways to educate people in rural areas with verified health information and motivate them to adopt prescribed health behaviors. Despite minimal internet access in rural areas of Bangladesh and India, about 94% of rural Bangladeshi households own at least one mobile phone and 90% of the Indian population has mobile phone subscriptions. Mobile phone users often receive mass text messages on COVID-19 issues from the government, urging users to practice social distancing and good hygiene. However, many people struggle to understand text messages due to high illiteracy among adults in rural areas, which often makes text messages an ineffective method of communication with rural people.
Design
To raise awareness about COVID-19 and preventative measures, a telephone-based health information campaign was carried out between early-April and mid-May 2020 in rural communities of Bangladesh (Khulna and Satkhira districts) and India (Kanpur of Uttar Pradesh). Rural households in Bangladesh and India were randomly selected from a larger pool previously surveyed by a partner NGO and one adult was asked to participate in the intervention. More than 8100 Participating households from 460 villages were randomly assigned to receive one of three forms of the intervention:
- Text-messages only: Each participant received a carefully written message about COVID-19 preventative measures. This message was sent again as a reminder after one month.
- Phone calls only: Each participant received two personal phone calls from the NGO to briefly discuss (for 10-15 minutes) the COVID-19 preventative measures and also to answer any queries about COVID-19 they might have. The first call followed a carefully crafted script; during the second, callers engaged in conversations related to the current COVID-19 situation, the importance of compliance with prescribed measures, and responded to queries made by respondents. This was to avoid repetition and make the discussions more engaging and natural.
- Both text-messages and phone calls: Each participant received two phone calls and two text-messages. Phone calls were always made 2-3 days after sending text-messages so that recipients would have time to read them and callers could refer back to them to facilitate conversation.
All phone calls and text-messages were personalized, addressed to the recipient’s full name, and the content was developed following WHO and national directives for the respective countries. The one-on-one phone calls served to increase the salience of prescriptive norms around COVID-19 and help people understand, remember, and act on the messages received.

NGO workers making phone calls
Impact
In a randomized evaluation, communicating information via both text-messages and phone calls was most effective at improving people’s compliance with prescribed health guidelines one month after the campaign, followed by phone calls alone. When compared to those who received only text-messages, both groups reported compliance between 1-1.5 standard deviations higher in Bangladesh and between 2.2-2.7 standard deviations higher in India on an index of compliance with public health guidelines. A second survey with a subset of women participants in Bangladesh revealed that the impact on compliance persists after three months.
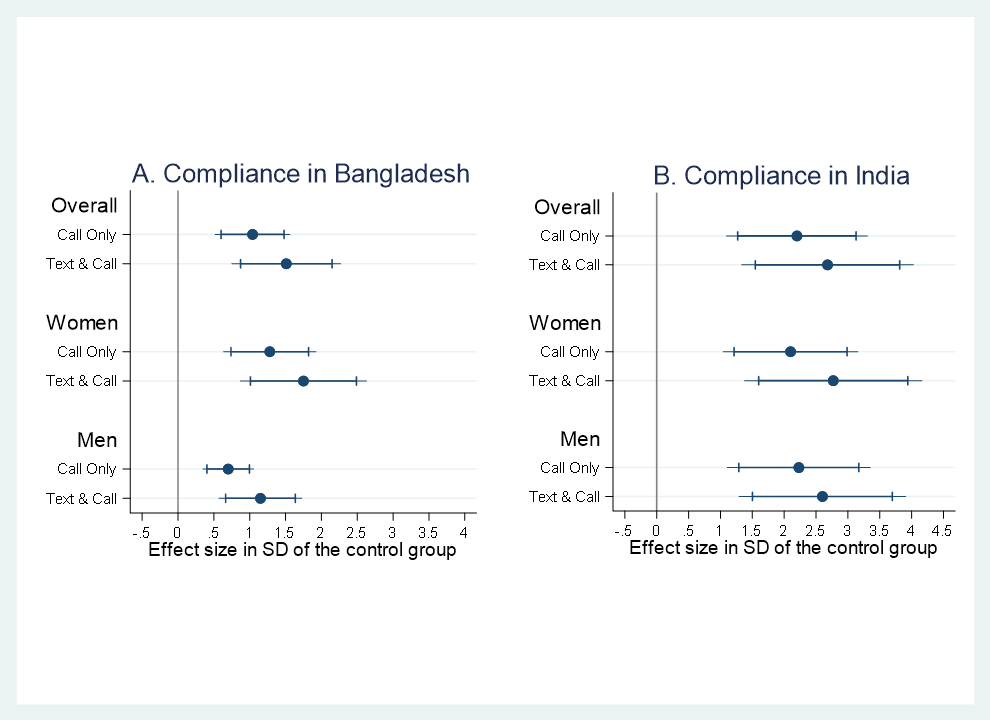
Treatment effects on compliance, pooled and by gender with 99% and 95% CIs. Control group = text only.
The interventions that included phone calls had greater impact on women’s compliance with health protective measures than men, and with a more pronounced effect in Bangladesh. Further analysis suggests that concern over the health of the family motivates women to be more compliant with health guidelines than men.
These findings suggest that communicating evidence-based health messages via brief telephone conversations can significantly enhance people’s awareness and compliance with COVID-19 precautionary measures.
Implementation Guidelines
Inspired to implement this design in your own work? Here are some things to think about before you get started:
- Are the behavioral drivers to the problem you are trying to solve similar to the ones described in the challenge section of this project?
- Is it feasible to adapt the design to address your problem?
- Could there be structural barriers at play that might keep the design from having the desired effect?
- Finally, we encourage you to make sure you monitor, test and take steps to iterate on designs often when either adapting them to a new context or scaling up to make sure they’re effective.
Additionally, consider the following insights from the design’s researchers:
- Callers were recruited locally by NGOs and were experienced in conducting interviews over the phone. Additionally, they received training for the effective delivery of health messages by phone. The call scripts were developed by one of the project researchers and reviewed by the research team. The scripts also included specific guidelines on content delivery and questions about members of the household. Callers were asked to spend at least 5 minutes talking to each person and to make sure that they have listed to understand everything said. Each phone call lasted for about 10 minutes.
- Researchers relied on self-reported measures of compliance because other outcome measures, such as coronavirus testing and infection rates, are often not available and likely underestimated when available for rural areas due to lack of testing and limited testing facilities in rural areas. Also, location and mobility data through smartphones were not feasible due to a lack of smartphone use and limited internet access in rural areas.
- Compliance with COVID-19 public health guidelines was measured by asking respondents how often they left home in the past week to (i) go to the market, (ii) visit doctors, (iii) for entertainment purposes (e.g., to attend weddings), (iv) for religious purpose (i.e., to offer prayers), (v) how often they washed their hands, and (vi) how often they did not hug or shake hands with outsiders in the past week. Questions were answered on a 6-point scale: 0=Did not go outside, 1=one day, 2=two days, 3=three days, 4=five days, 5=Every day. Responses were coded into indicators of compliance (0-2 complied, and 3-5 did not comply). Using the 6 activity indicators, a standardized compliance index was created.
Project Credits
Researchers:
Abu Siddique Technical University of Munich
Tabassum Rahman University of Newcastle
Debayan Pakrashi Indian Institute of Technology Kanpur
Asad Islam Monash University
Firoz Ahmed Khulna University