Defaults Guide End-of-Life Care
Organization : Center for Health Incentives and Behavioral Economics
Project Overview
Project Summary
Patients submitted advance directives (a written statement of a person’s wishes regarding medical treatment) on which they were required them to choose whether they wanted comfort-oriented or life-extending care. One of the options was already marked with an “X.”
Impact
A randomized evaluation found that people’s selections varied based on which option was preselected. When neither option was preselected on the advance directive, 61% of patients chose comfort-oriented care. When comfort-oriented care was preselected on their advance directive, 77% of patients opted for it. Just 43% of patients who received advance directives with life-extending care as the default option chose comfort-oriented care.
Challenge
When a patient fills out an advance directive—a statement of their medical wishes should they be unable to communicate them to a doctor—those choices will have large effects on their experience in hospice care, should they need it. However, something very small can have an effect on a big decision: the way the options are displayed on the form can influence whether they choose life-extending or comfort-oriented care. Insights from behavioral science can help inform choice structure to ensure that patients receive the most appropriate care.
Design
Patients completed one of three advance directives that required them to choose the type of end-of-life care they preferred. All the forms contained the same options, but some included a default, marking a particular type of care with an “X.” Patients could choose to keep the default selection or change it. The forms either preselected comfort-oriented care, life-extending care, or neither.
Impact
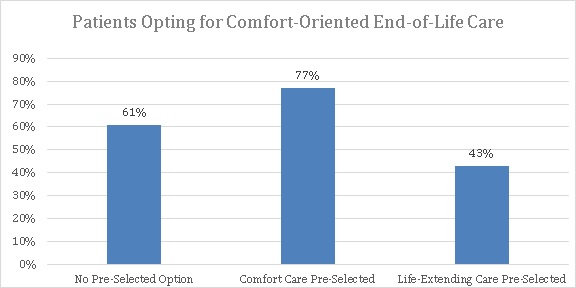
A randomized evaluation found that presenting patients with a default, preselected influenced the type of end-of-life care patients chose. When the advance directed had no preselected option, 61% percent of patients chose comfort-oriented care. Of patients who received an advance directive with comfort-oriented care marked, 77% kept that default option, while just 43% of patients chose comfort-oriented when life-extending care was already marked as the default.
Implementation Guidelines
Inspired to implement this design in your own work? Here are some things to think about before you get started:
- Are the behavioral drivers to the problem you are trying to solve similar to the ones described in the challenge section of this project?
- Is it feasible to adapt the design to address your problem?
- Could there be structural barriers at play that might keep the design from having the desired effect?
- Finally, we encourage you to make sure you monitor, test and take steps to iterate on designs often when either adapting them to a new context or scaling up to make sure they’re effective.
Additionally, consider the following insights from the design’s researcher:
- It should be easy for patients to choose the alternative care option that is not preselected.
Project Credits
Researchers:
Scott Halpern Contact University of Pennsylvania
George Lowenstein Carnegie Mellon University
Kevin Volpp The Wharton School at University of Pennsylvania; Leonard Davis Institute of Health Economics
Elizabeth Cooney Fostering Improvement in End-of-Life Decision Science Program
Kelly Vranas Philadelphia Veterans Affairs Medical Center
Caroline Quill Hospital of the University of Pennsylvania
Mary McKenzie Hospital of the University of Pennsylvania
Michael Harhay University of Pennsylvania
Nicole Gabler University of Pennsylvania
Tatiana Silva University of Mannheim
Robert Arnold University of Pittsburgh
Derek Angus University of Pittsburgh
Cindy Bryce University of Pittsburgh