Improving Sleep Apnea Treatment
Organization : Center for Health Incentives and Behavioral Economics
Project Overview
Project Summary
Patients received web-based access to their daily usage of the treatment for 3 months.
Impact
A 1.2 hour increase in daily usage of the medical treatment, from a starting average of 4.7 hours of daily use.
Source
Source
Challenge
Obstructive sleep apnea (OSA) is the repetitive closure of airways during sleep and is associated with increased morbidity and mortality. OSA has both health and functional effects, such as increased risk of heart attack and lower job performance. Positive airway pressure (PAP) is the medical treatment for OSA, but only about half of all patients use PAP for four or more hours per day, which is the minimum threshold for adequate use.
Design
Patients with newly diagnosed obstructive sleep apnea (OSA) starting positive airway pressure (PAP) treatment received usual follow-up care at their sleep centers, along with web-based access to data on their own PAP usage which was updated daily on a website called Way to Health.
Participants with web-based access to this data could log onto the site at any time during the three-month period to view their daily hours of PAP use (i.e. how long they wore their mask) displayed in both numerical and bar graphs. When they logged on, the website prompted them to indicate (yes/no) if they had used the PAP treatment for at least 4 hours in the past day to verify that they had logged on.
Impact
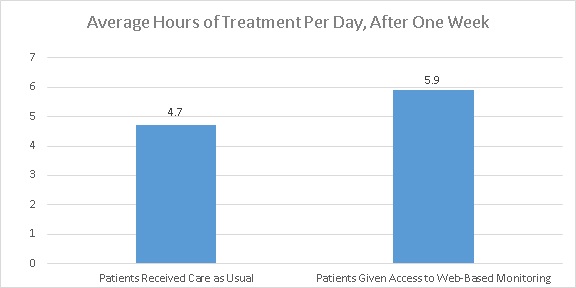
A randomized evaluation found that, during the first week of treatment, patients in two web-access groups used the PAP mask for a daily average of 5.9 hours and 6.3 hours respectively. Their adherence to the treatment was significantly better than that of patients in the usual care group, who averaged 4.7 hours of daily use.
Patients who were offered financial incentives in addition to the access to their data were more likely to log on to the site, but were not any more likely to adhere to their treatment than patients who were simply provided with online access to their personal data.
Over three months, adherence to the treatment decreased at a relatively constant rate in all three groups. Average daily use over the 3-month period was 3.8 hours in the usual care group, 4.8 hours in the web access group, and 5.0 hours in the web access plus financial incentive group.
The results suggest that giving patients access to their own treatment data can improve patient engagement and adherence to care regimens.
Implementation Guidelines
Inspired to implement this design in your own work? Here are some things to think about before you get started:
- Are the behavioral drivers to the problem you are trying to solve similar to the ones described in the challenge section of this project?
- Is it feasible to adapt the design to address your problem?
- Could there be structural barriers at play that might keep the design from having the desired effect?
- Finally, we encourage you to make sure you monitor, test and take steps to iterate on designs often when either adapting them to a new context or scaling up to make sure they’re effective.
Project Credits
Researchers:
Samuel T. Kuna Perelman School of Medicine, University of Pennsylvania
David Shuttleworth Leonard Davis Institute Center for Health Incentives and Behavioral Economics
Lugi Chi Lankenau Medical Center
Sharon Schutte-Rodin Perelman School of Medicine at the University of Pennsylvania
Eliot Friedman Paoli Hospital
Hengyi Guo Perelman School of Medicine at the University of Pennsylvania
Sandeep Dhand Holy Redeemer Hospital
Lin Yang Leonard Davis Institute Center for Health Incentives and Behavioral Economics
Jingsan Zhu Leonard Davis Institute Center for Health Incentives and Behavioral Economics
Scarlett L. Bellamy Perelman School of Medicine, University of Pennsylvania
Kevin G. Volpp Wharton School, University of Pennsylvania
David A. Asch Wharton School, University of Pennsylvania